Introduction
This policy applies to all persons working for us or on our behalf in any capacity, including employees at all levels, Directors, Senior Managers, Agency Workers, Locums and Suppliers. We strictly prohibit the use of modern slavery and human trafficking in our services and supply chain. We have and will continue to be committed to implementing systems and controls aimed at ensuring that modern slavery is not taking place anywhere within our organisation or in any of our supply chains. We expect suppliers to the same high standards.
Definitions
• Modern slavery
The Modern Slavery Act 2015 encompasses slavery, human trafficking, forced labour and domestic servitude. Traffickers and slave masters use whatever means they have at their disposal to coerce, deceive and force individuals into a life of abuse, servitude and inhumane treatment.
• Human Trafficking
Trafficking is the movement of people by means such as force, fraud, coercion or deception with the aim of exploiting them. It is a form of Modern Slavery. People can be trafficked for many different forms of exploitation such as forced prostitution, forced labour, forced begging, and forced criminality, forced marriage, domestic servitude and forced organ removal. Trafficking can occur within the UK as well as countries outside the UK.
Key signs of Modern Slavery and Human Trafficking
Physical
• Injuries apparently as a result of assault or controlling measures
• Neurological symptoms, headaches, memory loss, dizzy spells
• Gastrointestinal symptoms
• Cardiovascular symptoms
• Musculoskeletal symptoms
• Tattoos or other marks indicating ownership by exploiters
• Work related injuries, often through inadequate personal protective equipment or poor health and safety measures.
Sexual
• Sexually transmitted infections
• Injuries of a sexual nature
• Gynaecological symptoms such as urinary or virginal infections, pelvic inflammation
• Pregnancy as a result of their modern slavery situation, or they may have recently been forced to terminate a pregnancy.
Psychological
• Expression of fear or anxiety
• Depression or isolation
• Suffering from post-traumatic stress and or a range of other trauma induced mental or physical illnesses
• An attitude of self-blame, shame and an extensive loss of control
• Withdrawn and submissive
• Drug or alcohol use
• Self-harm
• Suicidal ideations.
• Reluctance to seek help
• Poor or no antenatal care
• Few personal effects.
Situational and environmental indicators
• Frequently moves locations, boroughs, counties, or countries
• Fearful or emotional about their family or dependants
• Lack of knowledge about the area they live in the UK
• Passport or travel document has been confiscated
• Fear of saying what their immigration status is
• Limited English, e.g., having vocabulary relating only to their exploitative situation
• Acting as if instructed by another
• Someone is taking advantage of their illegal status in the UK
• Distrust of authorities.
General Signs
• No passports
• No information about rights as a UK worker
• No information about their rights as a visitor in the UK
• Vague and inconsistent history
• Always accompanied by someone who may appear controlling
• Person with them does all the talking
• Never left alone
• Unsure of own medical history
• Not registered with a GP, nursery or school
• Appearance suggest neglect, note, someone working in prostitution may look well kept.
What to do if you spot the signs
If you suspect that a person is a victim of slavery or trafficking, this is a safeguarding issue. You should trust and act on your professional instinct that something is not quite right. It is usually a combination of triggers, an inconsistent story and a pattern of symptoms that may cause you to suspect trafficking. If you have any concerns about a child, young person or adult take immediate action to ask further questions and get additional information and support. It is important to remember that:
- trafficked people may not self-identify as victims of modern slavery
- trafficking victims can be prevented from revealing their experience to health care staff from fear, shame, language barriers and a lack of opportunity to do so. It can take time for a person to feel safe enough to open up
- err on the side of caution regarding age. If a person tells you they are under 18 or if a person says they are an adult, but you suspect they are not, then take action as though they were under 18 years old
- support for victims of human trafficking is available
Action to take
- Take immediate action for those considered to be in immediate danger
- Follow local safeguarding referral processes
- Raise concerns with safeguarding lead
- Ensure a clear and accurate record of the concern is made and actions taken.
Policy
Commitments
We are a company that expects everyone working with us or on our behalf to support and uphold the following measures to safeguard against modern slavery and human trafficking:
- We have a zero-tolerance approach to modern slavery and human trafficking in our organisation and our supply chains.
- The prevention, detection and reporting of modern slavery and human trafficking in any part of our organisation or supply chain is the responsibility of all those working for us or on our behalf. Colleagues must not engage in, facilitate or fail to report any activity that might lead to, or suggest, a breach of this policy.
- We are committed to engaging with our stakeholders and suppliers to address the risk of modern slavery and human trafficking in our operations and supply chain.
- We take a risk-based approach to our contracting processes and keep them under review. We assess whether the circumstances warrant the inclusion of specific prohibitions against the use of modern slavery and trafficked labour in our contracts with third parties. Using our risked based approach, we will also assess the merits of writing to suppliers requiring them to comply with our Code of Conduct, which sets out the minimum standards required to combat modern slavery and human trafficking.
Consistent with our risk-based approach we may require:
- Employment and recruitment agencies and other third parties supplying workers to our organisation to confirm their compliance with our Code of Conduct.
- Suppliers engaging workers through a third party to obtain that third parties’ agreement to adhere to the Code.
As part of our ongoing risk assessment and due diligence processes, we will consider whether circumstances warrant us carrying out audits of suppliers for their compliance with our Code of Conduct.
If we find that other individuals or organisations working on our behalf have breached this policy, we will ensure that we take appropriate action. This may range from considering the possibility of breaches being remediated and whether that might represent the best outcome for those individuals impacted by the breach to terminating such relationship.
| Section |
Details |
| Author |
David Englefield |
| Document Approver |
Dr. Adeolu Arikawe |
| Staff Group |
Safeguarding Leads |
| Consultation |
[Insert Consultation Details] |
| Version |
V1.0 |
| Date Issued |
May 2025 |
| Review Date |
April 2026 |
| Review Frequency |
Annual |
| Reason for Review |
New policy |
Organisational Structure and Supply Chains
SPCL is a provider of Healthcare, whose registered office is in Leicester
We deliver healthcare services in Leicestershire and Warwickshire. We employ staff ranging from General Practitioners, NMC registered Nurses and administrative support staff. We procure goods and services from a range of providers. Contracts vary from small one-off purchases to service contracts.
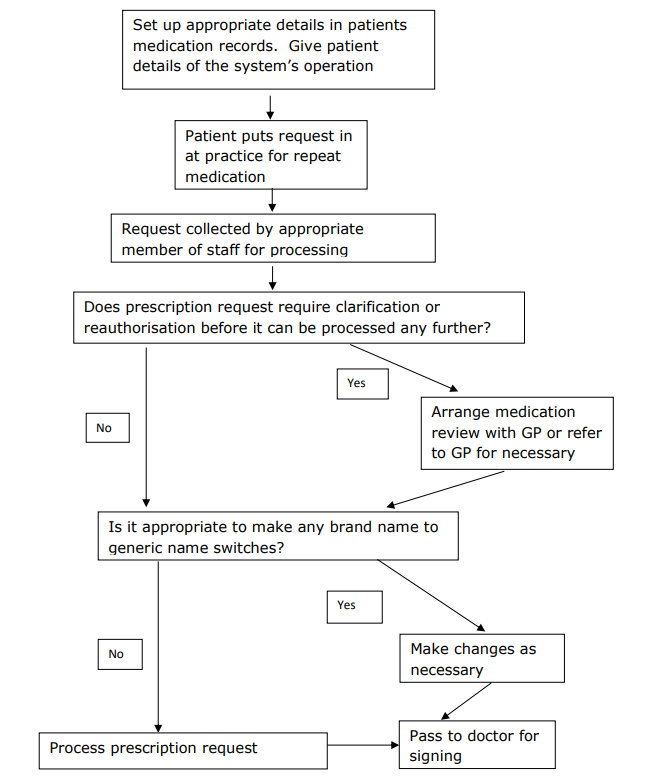
Our current Procurement processes are as below:
- All spend, aside from a few exceptions such as rates, is paid via PO. The Applicable Contract Terms Policy applies to any NHS organisation and states that where an NHS body issues a PO the standard Terms & Conditions apply.
- Our procurement process has been reviewed to ensure that human trafficking and modern slavery issues are considered at an early stage, requiring self-certification from potential suppliers that their supply chains comply with the law.
- We procure many goods and services through frameworks endorsed by the NHS, under which suppliers such as Crown Commercial Services and NHS Supply Chain adhere to a code of conduct on forced labour.
- We operate professional practices relating to procurement and supply and ensure procurement staff attend regular training on changes to procurement legislation.
- Due Diligence Processes for Slavery and Human Trafficking With regard to national or international supply chains, our point of contact is always preferably with UK entities, and we expect these to comply with legislation and have suitable anti-slavery and human trafficking policies and processes in place.
- The majority of our purchases utilise existing supply contracts or frameworks which have been negotiated under the NHS Standard Terms and Conditions of Contract, these all have the requirement for suppliers to have suitable anti-slavery and human trafficking policies and processes in place.
- Organisational policies in relation to slavery and human trafficking – We update relevant policies on a regular basis to highlight obligations where any issues of modern slavery or human trafficking might arise, particularly in our procedures for safeguarding adults and children and young people, tendering for goods and services, and recruitment and retention.
- Assessing and managing risk and due diligence processes in relation to slavery and human trafficking – We are committed to ensuring that there is no modern slavery or human trafficking in our supply chains or in any part of our business.
To identify and mitigate the risks of modern slavery and human trafficking in our own business and our supply chain we:
- adhere to the National NHS Employment Checks / Standards (this includes employees UK address, right to work in the UK and suitable references
- have systems to encourage the reporting of concerns and the protection of whistleblowers
- purchase a significant number of products through NHS Supply Chains, who’s ‘Supplier Code of Conduct’ includes a provision around forced labour. Other contracts are governed by standard NHS Terms & Conditions. High value contracts are effectively managed, and relationships built with suppliers
Effective action taken to address modern slavery – Performance Indicators
We are committed to social and environmental responsibility and have zero tolerance for Modern Slavery and Human Trafficking. Any identified concerns regarding Modern Slavery and Human Trafficking are escalated as part of the organisational safeguarding process. This statement is made pursuant to section 54(1) of the Modern Slavery Act 2015 and constitutes BWPCAs slavery and human trafficking statement for the current financial year.
Training for staff
All staff receive a comprehensive induction programme which includes information on, and guidance regarding, slavery and human trafficking. All staff are required, as part of mandatory training, to complete safeguarding courses, which cover obligations under the Act.
We also require external agencies supplying temporary staff to demonstrate compliance with the legislation. All clinical and non-clinical staff have a responsibility to consider issues regarding modern slavery and incorporate their understanding of these into their day-to-day practices.
All colleagues have a personal responsibility for the successful prevention of slavery and human trafficking with the procurement department taking responsibility for overall compliance.
A quarterly Integrated Learning Report is submitted to the Board of Directors which includes an overview of the number of concerns raised by staff and the category that they fall into.
Signed
Managing Director – David Englefield
Clinical Lead – Dr Adeolu Arikawe